The Benefits of Neurorehabilitation for Parkinson’s Disease

What is Parkinson’s Disease?
Parkinson’s disease (PD) is a progressive neurological disorder that affects movement, balance, and motor function. Common symptoms include tremors, muscle rigidity, and impaired balance and coordination. While there is no cure for Parkinson’s, neurorehabilitation services can play a transformative role in managing symptoms, enhancing quality of life, and potentially slowing functional decline. Here’s a closer look at the key benefits of neurorehabilitation for clients diagnosed with Parkinson’s.
1. Improved Mobility and Balance
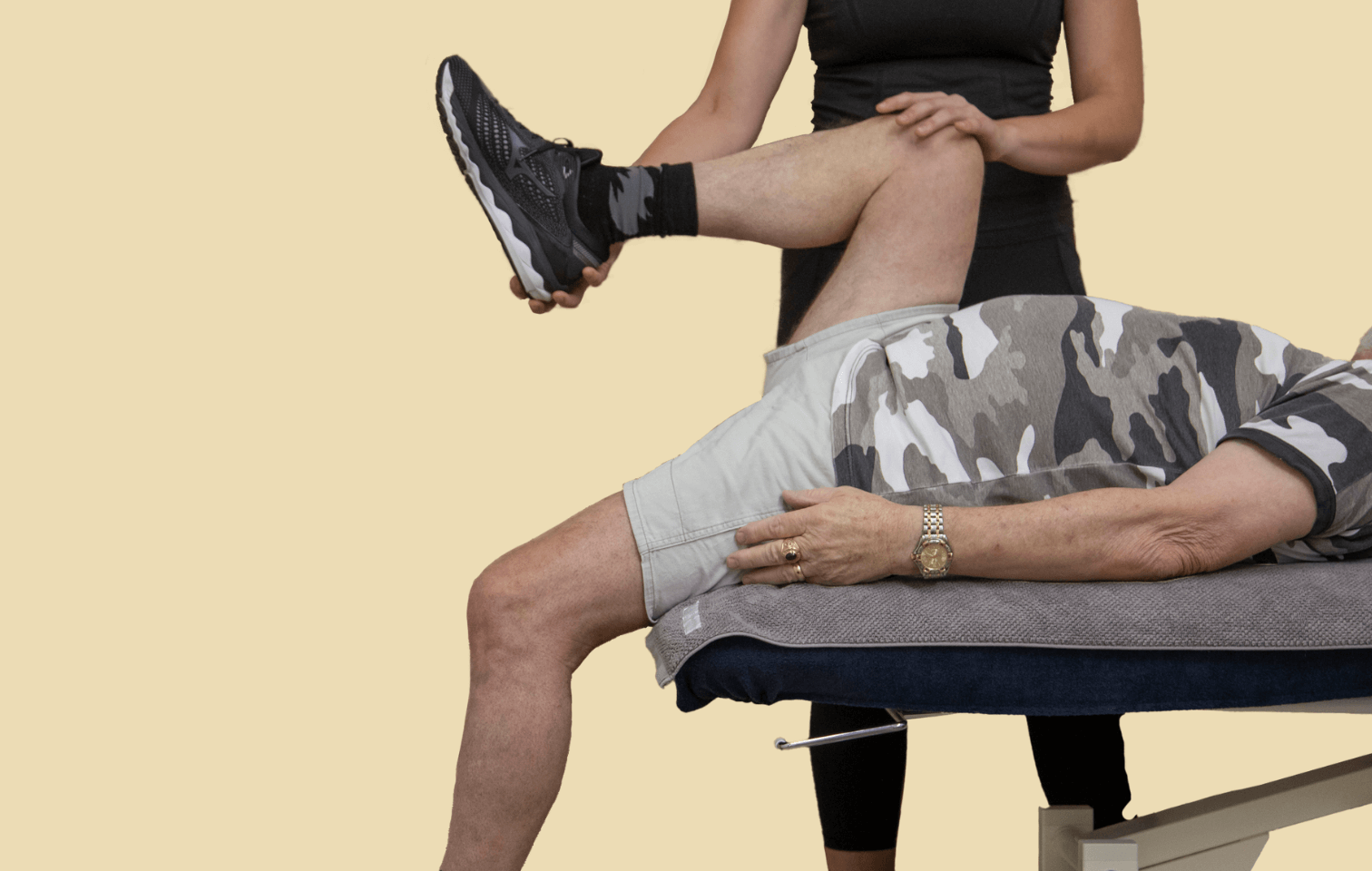
Neurorehabilitation combines therapeutic exercises tailored to a client’s specific needs to enhance motor function, which is often impaired in Parkinson’s. Physiotherapy, a core aspect of neurorehabilitation, focuses on exercises that target balance, posture, and coordination. This is crucial for clients with Parkinson’s, as their risk of falls is significantly higher than in the general population. Regular balance and gait training can help clients maintain a more stable and confident stride, reducing fall risk and supporting safe, independent movement.
2. Enhanced Strength and Flexibility
Muscle rigidity is a hallmark symptom of Parkinson’s, which can lead to stiffness and discomfort. Exercise physiology services in neurorehabilitation provide personalized strength training programs that help maintain muscle flexibility and strength. Building muscle strength and improving flexibility not only counteracts rigidity but also supports joint health, making movement more manageable and reducing the strain on clients’ muscles and joints over time.
3. Speech and Swallowing Support
As PD progresses, clients may experience difficulties with speech and swallowing, affecting both communication and nutrition. Speech therapy, an essential part of neurorehabilitation, addresses these issues by working on vocal strength, volume, articulation, and safe swallowing techniques. Strengthening these areas can improve communication and quality of life, helping clients maintain meaningful social interactions and a sense of normalcy in daily activities.
4. Better Management of Non-Motor Symptoms
Parkinson’s can also involve non-motor symptoms, such as mood changes, depression, and cognitive challenges. Neurorehabilitation often incorporates psychological and occupational therapy, which support clients in managing mental health symptoms and improving cognitive function. Mindfulness exercises, cognitive retraining, and coping strategies are common approaches that address these aspects of PD holistically, helping clients to maintain emotional resilience and cognitive skills.
5. Optimised Daily Functioning through Occupational Therapy
Occupational therapy is instrumental in teaching practical adaptations to manage everyday tasks. For clients with PD, this might mean learning ways to make dressing, cooking, or cleaning easier and safer. Occupational therapists also advise on home modifications, such as installing grab bars or using adaptive tools, making daily life simpler and allowing clients to maintain their independence longer.
6. Individualised Reformer Pilates for Posture and Core Strength
For many people with PD, core stability can be a significant challenge. Reformer Pilates, led by a trained neurorehabilitation professional, focuses on controlled movements that strengthen the core, improve posture, and build resilience in the body. These exercises can be highly beneficial for PD clients, especially in promoting stability and balance, which helps mitigate some of the mobility and postural difficulties associated with the disease.
7. Hydrotherapy for Low-Impact Rehabilitation
Water-based therapies, or hydrotherapy, offer a low-impact way for clients to exercise without excessive strain on muscles and joints. This form of rehabilitation is beneficial for Parkinson’s clients who may have limited mobility and struggle with land-based exercises. The buoyancy of water supports the body, reduces fear of falling, and allows clients to work on strength, coordination, and flexibility in a controlled, comfortable environment.
Benefits for Long-Term Disease Management
Incorporating neurorehabilitation into a client’s Parkinson’s care plan can be transformative in the long term. Regular participation in neurorehabilitation activities helps clients manage their symptoms more effectively and can potentially slow disease progression. Additionally, these services promote a sense of community and social support, which are essential for mental health and well-being. With neurorehabilitation, clients are empowered to regain control over their lives, set meaningful goals, and stay as active and independent as possible, despite the challenges of Parkinson’s.
Why Choose a Multidisciplinary Neurorehabilitation Approach?
Given the multifaceted nature of Parkinson’s disease, a multidisciplinary neurorehabilitation team, like the one at Hiya Health, can provide tailored, comprehensive care. Working with specialists in physiotherapy, exercise physiology, occupational therapy, dietetics, and more, clients receive care that addresses both physical and emotional aspects of PD. This holistic approach helps clients maximise their health outcomes, maintain functional abilities, and sustain their quality of life through effective, individualised care.
In conclusion, neurorehabilitation services offer Parkinson’s clients critical support to navigate the complexities of their condition. Whether it’s through improving mobility, enhancing mental resilience, or finding adaptive solutions for daily challenges, neurorehabilitation empowers individuals to lead fuller, more functional lives.
We’re here to help individuals on their journey towards neurological recovery
Our dedicated Neurological Rehabilitation Program, led by our team of experienced Physiotherapists, offers personalised care and evidence-based interventions to empower patients and optimise their outcomes. Book an appointment today.
Author: Meg Braithwaite
Subscribe to e-news
Receive the latest health tips and news straight to your inbox