Physiotherapy for Osteoarthritis

What is Osteoarthritis?
Osteoarthritis (OA) is the world’s leading cause of joint pain, and one of the highest causes of disability in adults globally. Osteoarthritis is one of the most researched musculoskeletal conditions globally, and this blog references international treatment guidelines for management of Osteoarthritis.
Osteoarthritis is a condition that affects our joints, whereby the cartilage that covers the end of the bones becomes thin and rough. Normally the smooth thick cartilage surface allows our bones to glide so our joints can move freely. As this cartilage becomes rougher, osteophytes can form, which can lead to a multitude of symptoms.
What symptoms may you experience from Osteoarthritis?
- Stiff / painful joints.
- Grinding sensation in joints.
- Joint swelling.
- Deep aching / sharp sensation in joints
- Loss of joint function in daily tasks.
Where can it affect?
OA can occur in any joint, but commonly it affects the shoulders, hips, knees and ankles.
Why does it happen?
In the vast majority of cases, there is no direct cause of OA. It often results from a combination of factors. We expect to see arthritic changes naturally in joints from our 30s onwards, but this does not always directly link to pain. More commonly, arthritic joints become problematic from 50 years old onwards, and can feel worse as we age naturally. OA is more common in females, and can be passed through families genetically. External factors that could trigger an arthritic joint include a bone injury near the joint, being overweight or leading an inactive lifestyle.
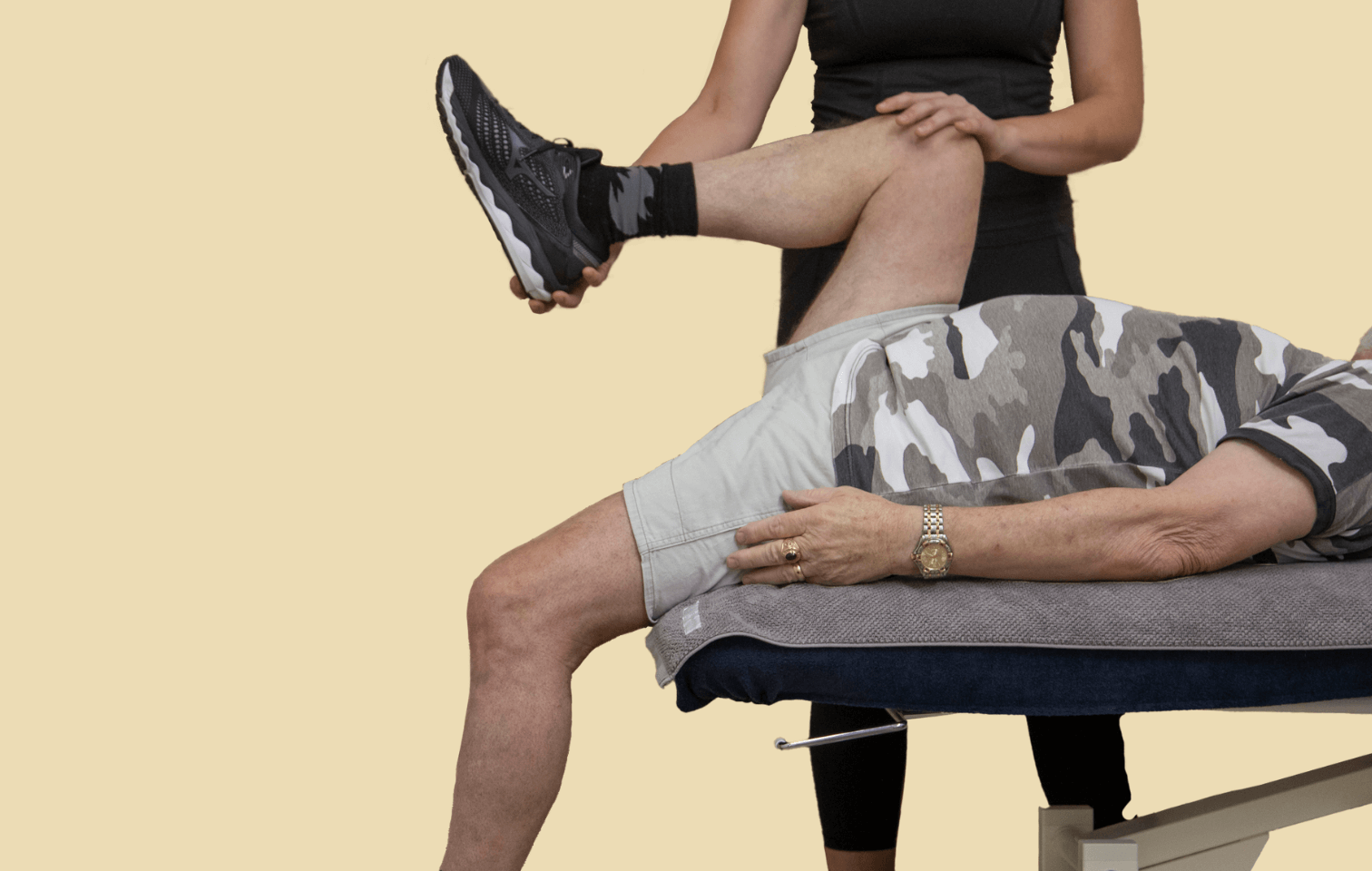
How can Physiotherapy and Exercise Physiology help?
The gold standard treatment for OA is education around its management, and exercise based therapy. Exercise is seen as the best form of non-surgical management of OA, and provides a multitude of other health benefits including increased muscle mass and joint strength, increased bone density and improved mood. This can be completed on land, but also in a hydrotherapy setting.
Strength exercise training has been shown to help the following:
- Improve joint shock absorbing capacity in the lower extremities.
- Improve joint pain management.
- Improve joint movement.
- Help maintain cartilage integrity.
At Hiya Health, our Physiotherapists can assist with a diagnosis of OA through a comprehensive assessment and treatment program, focusing on your individual needs and functional limitations. Alongside our Exercise Physiology team, we can help you with your short and long term management of OA if diagnosed, and overall help you improve your joint function, pain management and quality of life in daily tasks. Additionally if you are awaiting joint replacement surgery, we can treat you before and after surgery, to help you return to full function.
My experience as a Physiotherapist in treating osteoarthritis:
- Consistent progressive strength training significantly helps with symptom management and pain reduction. This can be in the gym, or our hydrotherapy pools.
- If you opt for joint replacement surgery, the importance of strength training before and after surgery cannot be understated – the stronger you are pre-surgery, the better your post-operative outcomes can be.
- Physiotherapists can help educate you on other pain management strategies to use alongside exercise based therapy, that can help alleviate your symptoms.
Tips & Self-Help Advice for Osteoarthritis
Incorporating some lifestyle changes, including stress management, exercise, stretching, activity modifications, nutrition and sleep health are all important factors in managing our symptoms and pain.
For example, some relaxation and good sleep health strategies can help, such as:
- Deep breathing exercises
- Progressive muscle relaxation
- Using pillows under knees, hips or legs can assist with pain reduction and improve comfort
Book an appointment with a physiotherapist today
If you are experiencing symptoms from Osteoarthritis, or believe you may need a diagnosis, the team at Hiya Health can help. Book an initial appointment today.


Author: Matt Chappell, Physiotherapist
References
Bannuru, R.R., Osani, M.C., Vaysbrot, E.E., Arden, N.K., Bennell, K., Bierma-Zeinstra, S.M.A., Kraus, V.B., Lohmander, L.S., Abbott, J.H., Bhandari, M. and Blanco, F.J., 2019. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis and cartilage, 27(11), pp.1578-1589.
Brosseau, L., Rahman, P., Toupin-April, K., Poitras, S., King, J., De Angelis, G., Loew, L., Casimiro, L., Paterson, G. and McEwan, J., 2014. A systematic critical appraisal for non-pharmacological management of osteoarthritis using the appraisal of guidelines research and evaluation II instrument. PloS one, 9(1), p.e82986.
Gränicher, P., Stöggl, T., Fucentese, S.F., Adelsberger, R. and Swanenburg, J., 2020. Preoperative exercise in patients undergoing total knee arthroplasty: a pilot randomized controlled trial.
Kolasinski, S.L., Neogi, T., Hochberg, M.C., Oatis, C., Guyatt, G., Block, J., Callahan, L., Copenhaver, C., Dodge, C., Felson, D. and Gellar, K., 2020. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis & rheumatology, 72(2), pp.220-233.
Messier, S.P., Mihalko, S.L., Beavers, D.P., Nicklas, B.J., DeVita, P., Carr, J.J., Hunter, D.J., Lyles, M., Guermazi, A., Bennell, K.L. and Loeser, R.F., 2021. Effect of High-Intensity Strength Training on Knee Pain and Knee Joint Compressive Forces Among Adults With Knee Osteoarthritis The START Randomized Clinical Trial. JAMA, 325(7), pp.646-657.
Walsh, N.E., Pearson, J. and Healey, E.L., 2017. Physiotherapy management of lower limb osteoarthritis. British Medical Bulletin, 1, p.11.
Subscribe to e-news
Receive the latest health tips and news straight to your inbox